- Early Onset Polymorphic Post-transplant Lymphoproliferative Disease Mimicking a Solitary Necrotizing Abscess in a Graft Liver
-
Pil Soo Sung, Jaejun Lee, Joon Lee, Hee Chul Nam, Si Hyun Bae, Seung Kew Yoon
-
J Liver Cancer. 2019;19(2):165-170. Published online September 30, 2019
-
DOI: https://doi.org/10.17998/jlc.19.2.165
-
-
 Abstract Abstract
 PDF PDF
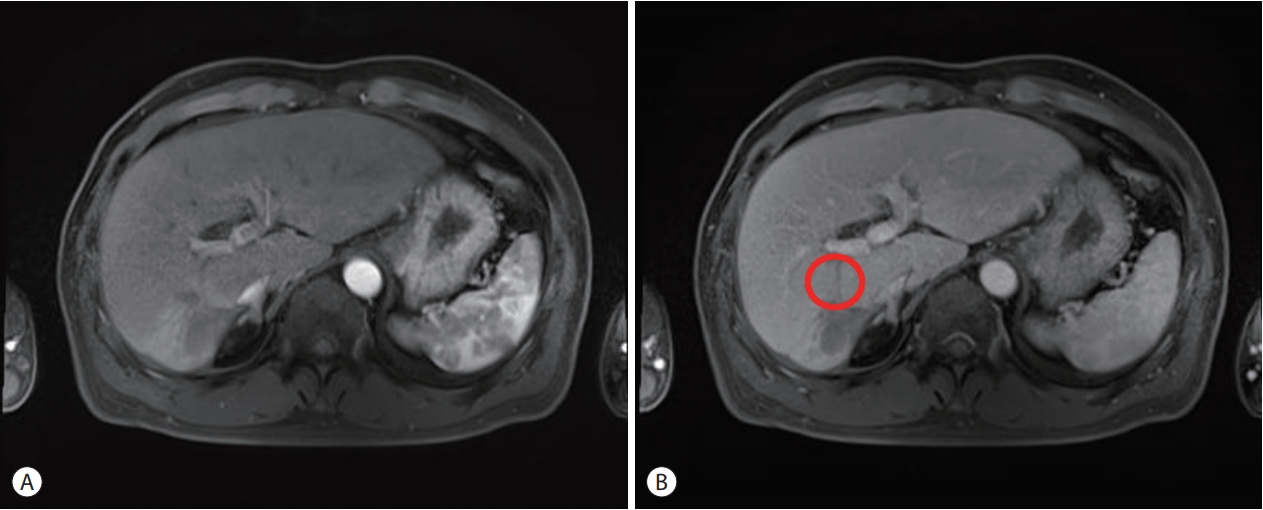
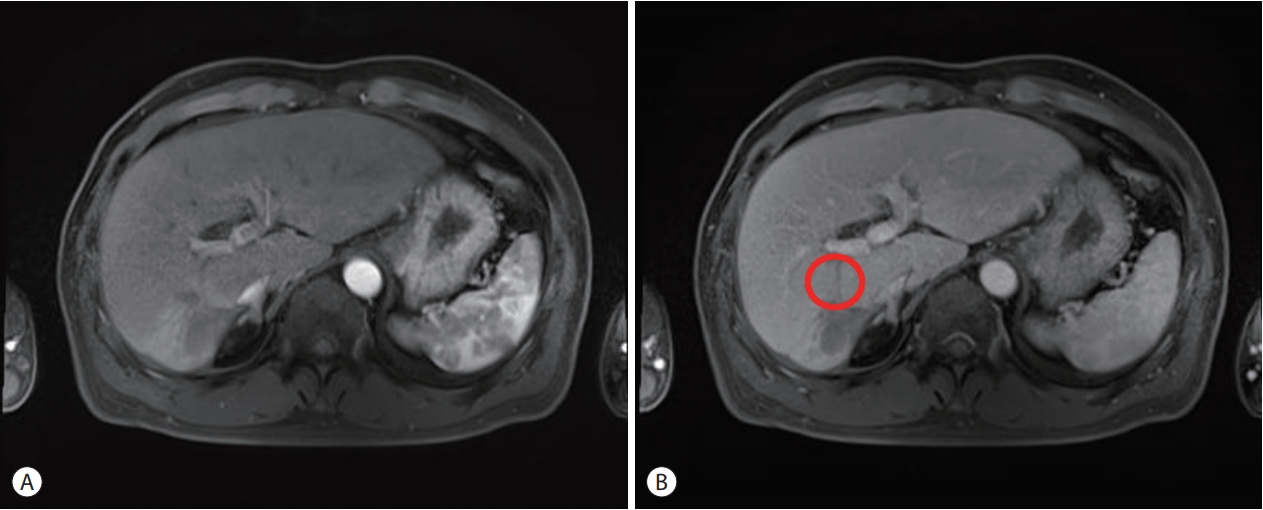
- Although post-transplantation lymphoproliferative disease (PTLD) after liver transplantation is very rare, its prognosis is worse than that of PTLD following other types of solid organ transplantation. Here, we report a rare case of early onset polymorphic PTLD in a graft liver occurring five months after deceased-donor liver transplantation due to hepatocellular carcinoma and hepatitis C virus infection. Initially, findings from contrast-enhanced magnetic resonance imaging mistakenly suspected the lesion was a necrotizing abscess with central necrosis. However, 18F-fluorodeoxyglucose positron emission tomography and biopsy findings confirmed an Epstein-Barr virus (EBV)-associated, B cell type polymorphic PTLD with central necrosis. Our case suggests regular monitoring of EBV serologic status for liver transplant recipients who were initially in an EBV seronegative state. Although early-onset PTLD is very rare after liver transplantation, PTLD should be suspected when recipients show the seroconversion for EBV proteins and the development of new tumors with various clinical presentations.
- Liver Transplantation after Successful Downstaging with Hepatic Arterial Infusion Chemotherapy in a Patient with Hepatocellular Carcinoma with Portal Vein Tumor Thrombus
-
Hee Chul Nam, Pil Soo Sung, Ho Jong Chun, Dong Goo Kim, Jeong Won Jang, Jong Young Choi, Seung Kew Yoon
-
J Liver Cancer. 2019;19(1):64-68. Published online March 31, 2019
-
DOI: https://doi.org/10.17998/jlc.19.1.64
-
-
 Abstract Abstract
 PDF PDF
- Hepatocellular carcinoma (HCC) is one of the most common cancers worldwide. The majority of patients with HCC are diagnosed at advanced disease stages with vascular invasion, where curative approaches are often not feasible. Currently, sorafenib is the only available standard therapy for HCC with portal vein tumor thrombosis (PVTT). However, in many cases, sorafenib therapy fails to achieve satisfactory results in clinical practice. We present a case of advanced HCC with PVTT that was treated with hepatic arterial infusion chemotherapy (HAIC) followed by liver transplantation. Three cycles of HAIC treatment resulted in necrotic changes in most of the tumors, and PVTT was reduced to an extent at which liver transplantation was possible. Further studies are required to determine the treatment strategies for advanced HCC with PVTT that can improve prognosis.
- Comparative Study between Metronomic Chemotherapy and Transarterial Chemoembolization in Patients with Child-Pugh Class B Advanced Hepatocellular Carcinoma
-
Hyun Yang, Myeong Jun Song, Hee Chul Nam, Hae Lim Lee, Sung Won Lee, Do Seon Song, Jeong Won Jang, Si Hyun Bae, Jong Yong Choi, Seung Kew Yoon
-
J Liver Cancer. 2015;15(2):92-99. Published online September 30, 2015
-
DOI: https://doi.org/10.17998/jlc.15.2.92
-
-
1,302
Views
-
7
Downloads
-
1
Citation
-
 Abstract Abstract
 PDF PDF
- Background/Aim
s: Metronomic (MET) chemotherapy is a treatment characterized by
frequent infusion of low doses of chemotherapeutic agent without extended break. The aim
of this study is to evaluate the efficacy of MET chemotherapy compared with transarterial
chemoembolization (TACE) in patients with child B class advanced hepatocellular carcinoma
(HCC).
Methods
Seventy-three patients with child B class advanced HCC were analyzed between
April, 2007 and August, 2013 according to two treatment groups: (i) MET chemotherapy group
(n=43, Epirubicin 35 mg/body surface area [BSA] every 4 weeks, and cisplatin 15 mg/BSA and
5-fluorouracil 50 mg/BSA weekly for 3 weeks) via an implantable port system with 1 week
break. (ii) TACE group (n=30, Adriamycin 20-50 mg) every 4 weeks. Primary endpoint was
overall survival (OS).
Results
The median survival times in the MET and TACE groups were 4.5 months and
3.1 months, respectively. The overall survival rate showed significantly better in the MET
treatment group than in the TACE group (P=0.039). When the factors affecting patient
OS were analyzed, MET chemotherapy (P=0.038, hazard ratio {HR} 0.538 [95% confidence
interval {CI} 0.299-0.967]) was independently associated with OS. Larger maximal tumor size,
extrahepatic metastasis and advanced stage also were significant factors for OS (P=0.009, HR
1.064 [95% CI 1.014-16.064]; P=0.014, HR 2.120 [95% CI 1.164-3.861]; P=0.019, HR 2.046 [95% CI
1.125-3.720], respectively).
Conclusions
MET chemotherapy showed survival benefit than TACE in patients with child
class B advanced HCC. Therefore, MET chemotherapy may be considered as a treatment
option for advanced HCC with poor liver function. (J Liver Cancer 2015;15:92-99)
-
Citations
Citations to this article as recorded by  - A comparative study of sorafenib and metronomic chemotherapy for Barcelona Clinic Liver Cancer-stage C hepatocellular carcinoma with poor liver function
Hyun Yang, Hyun Young Woo, Soon Kyu Lee, Ji Won Han, Bohyun Jang, Hee Chul Nam, Hae Lim Lee, Sung Won Lee, Do Seon Song, Myeong Jun Song, Jung Suk Oh, Ho Jong Chun, Jeong Won Jang, Angelo Lozada, Si Hyun Bae, Jong Young Choi, Seung Kew Yoon
Clinical and Molecular Hepatology.2017; 23(2): 128. CrossRef
|